Sexually transmitted infection (STI) trends in the United States reflect both good news and bad news, according to Sexually Transmitted Infections Surveillance, 2022, released by the Centers for Disease Control and Prevention (CDC) on January 30. While cases of chlamydia have leveled off after rising for decades, and gonorrhea cases have declined, syphilis cases—including congenital syphilis—continue to surge.
“The STI field has reached a tipping point,” said Laura Bachmann, MD, MPH, acting director of the CDC’s Division of STD Prevention. “We have long known that these infections are common, but we have not faced such severe effects of syphilis in decades. Recent public health emergencies diverted program resources and threatened the health of those already disproportionately affected by STIs. We must move now to pick up the pieces.”
. Today @CDCSTD released the 2022 #STI Surveillance Report ???? https://t.co/SzEkJn01xM
— Dr. Jono Mermin (@DrMerminCDC) January 30, 2024
Here are four highlights from the #STIreport @CDCgov: (1/5) pic.twitter.com/hMwIrq0Kyn
The news comes at a time when funding for STI and sexual health services is under pressure and the public health workforce has been cut, leading advocates to call for greater efforts from the federal government.
“The CDC’s latest STI data shows that our nation is facing a rapidly deteriorating public health crisis with real lives at stake, the National Coalition of STD Directors (NCSD) said in a statement. “STIs—especially syphilis—will continue to spiral out of control until the administration and Congress provide communities with the funding they need to provide the most basic screening, treatment and prevention services.”
STI Trends and Disparities
According to the latest data, the three major reportable bacterial STIs—chlamydia, gonorrhea and syphilis—rose by about 2% between 2018 and 2022, exceeding 2.5 million combined cases. There was a small (1%) decrease from 2021 to 2022, but data for the past few years are less reliable due to changes in STI testing during the early years of the COVID pandemic. The overall STI rate, or cases per 100,000 population, also remained roughly stable.

From Sexually Transmitted Infections Surveillance, 2022CDC
But the combined data hide the real news about specific STIs and disparities among population groups. Rates of all three STIs differ substantially according to sex, age, race/ethnicity, sexual orientation, HIV status and region of the country.

From Sexually Transmitted Infections Surveillance, 2022CDC
Chlamydia—the most common notifiable STI—was roughly stable between 2021 and 2022, with a slight 0.3% uptick, bringing the total to nearly 1.65 million cases. But the five-year trend shows a substantial 6% decline, driven by a 9% reduction among women.
Young people in their late teens and twenties accounted for more than half of chlamydia cases in 2022, with women having a greater than twofold higher rate than men. Black people (who make up about 13% of the U.S. population) had the highest chlamydia rate by a large margin, accounting for 28% of cases. American Indians/Alaska Natives also had a high rate. Native Hawaiians/Pacific Islanders and Latinos had higher rates than white people, while Asians had the lowest rate. States in the South had higher rates compared with other regions, though South Dakota had an exceptionally high rate of all three STIs.
From Sexually Transmitted Infections Surveillance, 2022CDC
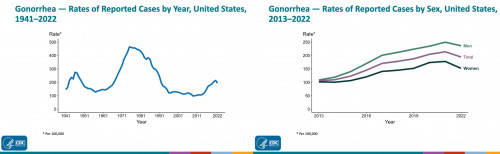
Gonorrhea, in contrast, decreased by about 5% among men and about 14% among women from 2021 to 2022, falling to about 648,000 total cases—the first decline in at least a decade. Despite this drop, the five-year trend still shows a 14% increase for men and a 6% rise for women. It is unclear why gonorrhea has declined even as syphilis cases have surged. Among gonorrhea cases tested for drug resistance in 2022, about half showed some degree of resistance to at least one antibiotic, but almost all circulating strains remain susceptible to ceftriaxone, the primary recommended treatment.
Young people also accounted for the largest share of gonorrhea cases, but here, men had a higher rate than women. In general, gay and bisexual men had a higher gonorrhea rate than heterosexual men and women—accounting for an estimated 36% of cases—but this varied by city and may be influenced by gay men’s greater likelihood of getting routine STI tests. Black people accounted for an even more disproportionate share of gonorrhea cases (38%) compared with chlamydia, and the other racial/ethnic groups followed the same ranking. Again, the states with the highest gonorrhea rates were concentrated in the South.

From Sexually Transmitted Infections Surveillance, 2022CDC
Syphilis saw the greatest increase of all the STIs, rising by 17% between 2021 and 2022 to reach 203,500 total cases. This contributed to a dramatic 80% jump over the past five years. In fact, syphilis numbers are higher today than they’ve been since the 1950s, and the upsurge has contributed to a shortage of one of the most effective antibiotics used for treatment.
The new data show that syphilis is not being diagnosed and treated in a timely manner. Left untreated, the bacteria can damage organs throughout the body, including the eyes, heart, bones and brain. From 2021 to 2022, cases of primary and secondary syphilis—the most infectious and most treatable stages—rose by 7% among men and by 20% among women, exceeding 59,000 cases. But late syphilis and syphilis of unknow duration increased even more—by 24% and 38%, respectively—reaching more than 87,500 cases. Since 2018, primary/secondary and late/unknown syphilis among women have risen by nearly 200%.

From Sexually Transmitted Infections Surveillance, 2022CDC
The epidemic of syphilis among young women has led to a parallel surge in congenital syphilis, which occurs when a mother transmits the bacteria during pregnancy or delivery. Congenital syphilis can cause miscarriages, stillbirths or premature births and can lead to serious complications for the baby, including neurological problems, blindness and deafness. Cases have climbed by 183% since 2018 and by more than 900% over the past decade. There was a 30% rise from 2021 to 2022 alone, reaching 3,755 cases and resulting in 282 stillbirths and infant deaths. Timely testing and treatment during pregnancy might have prevented nearly 90% of congenital syphilis cases, according to the CDC.
For primary/secondary syphilis, the age distribution was broader than for chlamydia and gonorrhea, and men had about a fourfold higher rate than women. Gay men accounted for the largest proportion of cases, at 29%, but heterosexual men and women are catching up. Nearly 40% of gay and bi men with primary/secondary syphilis were living with HIV. Black people accounted for about a third of primary/secondary syphilis and congenital syphilis cases, but Native Americans/Alaska Natives had by far the highest rates. States with high syphilis rates were scattered around the country, mainly in the South and West.
Curbing the STI Epidemic
Overall, half of chlamydia, gonorrhea and syphilis cases were among young people ages 15 to 24, and Black people accounted for about 30% of all STI cases. “[T]hese disparities are unlikely explained by differences in sexual behavior and rather reflect differential access to quality sexual health care, as well as differences in sexual network characteristics,” according to the report.
Health officials stress that more work is needed to address disparities in STI rates and to ensure equitable access to health services. All three STIs were much more likely to be diagnosed outside of STI clinics, underscoring the need for testing and treatment in primary care and other settings.
“We cannot continue to use decades-old prevention strategies to address today’s STI epidemic. People need testing and treatment to meet them where they are,” Bachmann said. “Some people face tremendous barriers to STI prevention and health services. So the most important work is often outside the clinic, whether it be reaching out to communities with testing, interviewing patients to offer services to their partners or delivering treatment directly to someone.”
Increased resources for STI prevention and other sexual health services are needed to curb the epidemic, experts and advocates say. Women’s sexual health services are especially threatened due to political contention around abortion. In some areas, facilities that offer abortion, such as Planned Parenthood clinics, are also key providers of other services, including STI prevention and treatment.
“[S]exual health services remain inadequate relative to the need pretty much everywhere,” but “it’s particularly a problem here in the United States,” Jay Varma, MD, of Siga Technologies, a former deputy commissioner of health for New York City, told the New York Times. “When you miss one case, you then end up with two more cases, and if you miss two cases, you then end up with four….That’s how epidemics grow.”
Fortunately, there’s a new tool in the STI prevention toolbox, at least for gay and bisexual men and transgender women. Studies have shown that taking a single dose of the antibiotic doxycycline within 72 hours after sex—known as doxyPEP—can reduce the risk of chlamydia and syphilis for these groups by around 70% to 90% and the risk of gonorrhea by 50% to 60%. DoxyPEP did not significantly reduce STI rates in a study of young women in Africa, but this approach still might work for those who achieve good adherence. The CDC issued the first doxyPEP guidelines in October.
“In the United States, syphilis was close to elimination in the 1990s, so we know it’s possible to reverse this epidemic,” said Jonathan Mermin, MD, MPH, director of the CDC’s National Center for HIV, Viral Hepatitis, STD and TB Prevention. “I have hope for innovative prevention tools—such as a pill after sex that prevents STIs and better tests for syphilis—but they will only be successful if they reach the people who will benefit.”
Click here to read the full Sexually Transmitted Infections Surveillance, 2022 report.







Comments
Comments