With the emergence during the current decade of new, highly effective treatments for hepatitis C virus (HCV), the future has looked rosier for the effort to combat the epidemic. While often inaccessible due to their astronomical expense, direct-acting antiviral (DAA) regimens have nevertheless afforded many people who had been living with the virus, oftentimes for decades—some three-quarters of the estimated 3.5 million U.S. residents who have HCV are baby boomers—the chance to finally rid their bodies of the insidious infection and to lower their risk of severe liver disease in particular.
Creeping up behind this optimistic front, however, has been the opioid epidemic’s own insidious expansion. As a sizable proportion of those who have developed opioid use disorder through the use of prescription pills has migrated to cheaper, more readily available heroin or other injectable opioids, the sharing of injection equipment among them has fueled a recent rise in HCV infection rates. (The opioid scourge may also have already reversed nearly two decades of declines of HIV transmission among people who inject drugs, or PWID.)
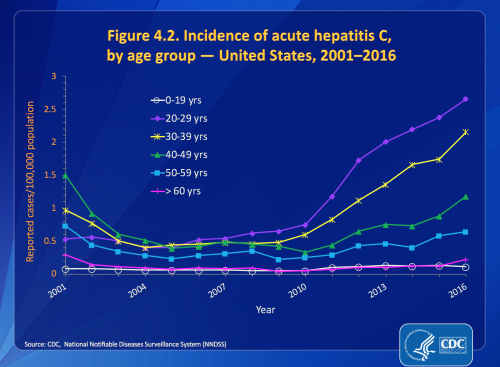
“Unfortunately, the opioid crisis is allowing hepatitis C to gain a foothold among a new generation of Americans at an alarming rate,” says Paul Weidle, PharmD, MPH, acting director of the Centers for Disease Control and Prevention’s (CDC) Division of Viral Hepatitis. “In 2016, the highest overall number and rates of new hepatitis C infections were among people ages 20 to 29.”
That year, an estimated 41,200 U.S. residents contracted hep C, a 21 percent one-year increase in the infection rate since 2015 and a three-and-a-half-fold surge since the beginning of the decade. Because the national surveillance system is so inadequate and patchy, and because HCV so often goes undiagnosed, the CDC must extrapolate such transmission figures from a quite limited data set; just under 3,000 new cases of the virus were actually reported in 2016, with data coming from only 42 states.
A recent CDC analysis charting the HCV epidemic’s expansion between 2005 and 2016 found that the annual diagnosis rate of acute cases of the virus—those diagnosed soon after infection—increased nearly seven-fold among 18- to 29-year-olds, from 0.4 cases to 2.7 cases per 100,000 people in this age bracket. At the same time, the acute-HCV diagnosis rate increased some five-and-a-half-fold among thirtysomethings, from 0.4 cases to 2.2 cases per 100,000 people.

Source: CDC
Source: CDC
Among the four largest racial groups in the United States—whites, Latinos, Blacks and Asians and Pacific Islanders—such increases in HCV diagnosis have been most pronounced among whites, in particular those living in nonurban areas; Appalachian, Midwestern and New England states have been the most affected. That said, Native Americans and Alaska Natives have far and away the greatest acute-HCV diagnosis rate of any racial group, one that was about three times greater than that of whites in 2016.
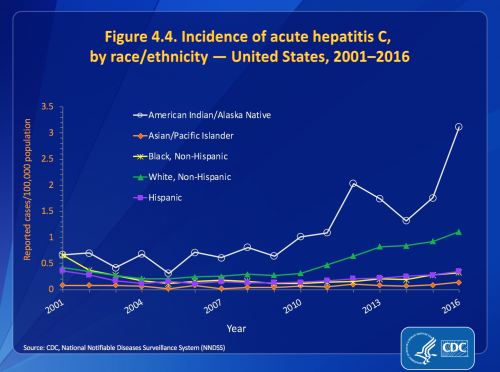
Source: CDC
Strong signs have pointed toward injection drug use as the driver of such upward trajectories in HCV infections, with the rate of admission to substance abuse programs for injection of prescription opioids expanding a respective nine-fold among 18- to 29-year-olds and nearly three-fold among 30- to 39-year-olds between 2004 and 2014, while admissions to such programs for heroin injection rose by a respective seven-fold and by about 80 percent in the two age brackets.
There is also an emerging epidemic, albeit a relatively small one, of sexually transmitted HCV among men who have sex with men in Western nations, in particular those who are living with HIV. Unsterilized tattooing is another mode of transmission for hep C.
About three quarters to 85 percent of those who contract hep C will develop a chronic infection—the remaining individuals spontaneously clear the virus—that can linger in the body for many years without causing any symptoms. Perhaps half of those currently living with chronic HCV in the United States are unaware of their infection, which over the course of decades can cause progressive liver damage and may lead to cirrhosis, liver cancer and the need for a transplant of the organ.
Hep C’s expansion among young people is of particular concern because of the risk it poses to babies born to expectant mothers who have the virus. Hep C transmits to the newborn in approximately 6 percent of such pregnancies or during childbirth, a figure that about doubles in women coinfected with HCV and HIV and also in those who have a high hep C viral load. There is no approved treatment that prevents such mother-to-child transmission of HCV, as there is for HIV.

Istock (Model(s) used for illustrative purposes only)
CDC researchers found that between 2011 and 2014, the rate of women of childbearing age—those 15 to 45 years old—who tested positive for HCV rose 22 percent, from 139 to 169 per 100,000 women in this age group. During that time, the proportion of all newborns whose mothers had HCV jumped by 68 percent, from 0.19 percent to 0.32 percent.
Weidle notes that children with hep C must wait until they are 12 years old to become eligible for DAA treatment. “The good news is that, for the most part, hepatitis C doesn’t cause serious disease in early childhood,” he adds. “Still, children that test positive who are in unstable situations or enter foster care may face an additional hurdle when it comes to medical follow-up.”
On top of recommending a one-time HCV screen for all baby boomers—those born between 1945 and 1965—the CDC urges individuals with a history of injection drug use to get tested for the virus, repeatedly if such behavior is ongoing. Additionally, the federal health agency stresses that health care providers should assess for hep C risk among their female patients of childbearing age, in particular those who are pregnant. All babies born to women with hep C should receive testing as well.

Istock
As for grappling with the swelling injection-drug-use epidemic, the CDC calls for expanded access to community-based drug-prevention programs that can give the opportunity for treatment and recovery services to people with substance-use disorders. Vital are the establishment of syringe services programs (SSPs), which provide clean drug-injection equipment to PWID.
“SSPs can play an important role in preventing hepatitis C infection, as well as providing a touchpoint for people at risk of infection to receive testing and enter care,” Weidle says. “However, this can only happen if people at risk for infection from injection drug use can access SSPs, which can be particularly challenging in rural areas.”
In fact, the CDC has found 80 percent of young people with hep C live more than 10 miles from an SSP. The median distance was 37 miles, with those living in rural areas and in Southern and Midwestern states burdened with further to travel.
Conservative politics often stymie the establishment of SSPs, with tough-on-crime lawmakers wary about giving the impression they are condoning injection drug use. In a notorious recent case, Indiana’s then-Governor Mike Pence crucially delayed the establishment of an SSP in Scott County, Indiana, despite warnings dating back years of the beginnings of a dual HCV-HIV outbreak among local PWID. A recent paper focusing on the HIV aspect of the outbreak estimated that if the state government had established a response to the emerging epidemic in 2011, including setting up an SSP, this could have averted almost all of the more than 200 new cases of that virus that ultimately were transmitted by 2015.
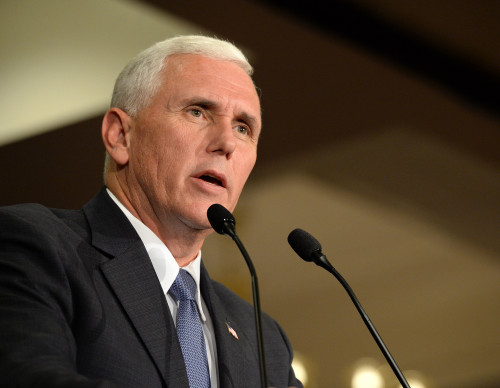
Mike PenceGino Santa Maria/Shutterstock.com
Seeking to prevent other Scott County–type outbreaks, the CDC warned 220 U.S. counties in 2016 that they are at risk of major clusters of HIV and HCV infections among local PWID. Sure enough, there have recently been reports of smaller outbreaks in Ohio, Kentucky, West Virginia, Massachusetts and Seattle.
Benjamin Ryan is POZ’s editor at large, responsible for HIV science reporting. His work has also appeared in The New York Times, New York, The Nation, The Atlantic and The Marshall Project. Follow him on Facebook, Twitter and on his website, benryan.net.







Comments
Comments